Improving prescribing in general practice at scale

Researchers from Yorkshire and Humber ARC teamed up with NHS West Yorkshire Integrated Care Board (ICB) to develop and deliver an evidence-based campaign to improve prescribing in general practice
Their continuing programme has targeted key NHS priorities, including antibiotic stewardship, reducing opioid prescribing and promoting greener, more effective use of asthma inhalers. It has now reached over 1000 practices across Yorkshire and Humber and North East England over the past five years.
General practice is responsible for half (or around £9 billion) of the total NHS medicines budget. Whilst many prescribed medicines help patients, a large number of prescriptions are for medicines that patients don’t need and that can actually cause harms.
The ARC team, led by Sarah Alderson and Robbie Foy, academic GPs at the University of Leeds, had completed two earlier studies showing that giving general practices regular feedback reduced harmful prescribing and saved money. The first study, funded by NIHR, targeted ‘high risk’ prescribing of medicines that can cause kidney damage and stomach bleeds. The second study evaluated the Campaign to Reduce Opioid Prescribing (CROP). Opioids are widely prescribed for people with long-term (chronic) pain. These morphine-based medicines generally don’t work for long-term pain and can result in addiction, dependency and an increased risk of falls and early death.
The ARC supported the scaling up of evidence-based feedback, which was positively received by general practices, and adaptation to tackle further problematic prescribing. CROP has since been run elsewhere, with similar benefits, including a 1.9% decline in overall opioid prescribing and 1.5% decline in strong opioid prescribing in South Yorkshire and Bassetlaw over 2021-22.
Effective antibiotic stewardship
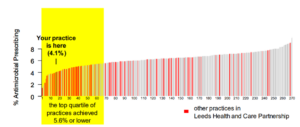
The resulting Lowering Anti-Microbial Prescribing (LAMP) campaign has been sustained since 2019. Tackling antibiotic resistance is a major global health challenge. Overusing antibiotics in healthcare leads to drug resistance, meaning these vital medicines stop working. Most antibiotics are prescribed in primary care settings like general practices. LAMP provides general practices with regular feedback comparing their antibiotic prescribing rates to other practices. This prompts them to reflect on and reduce unnecessary antibiotic prescribing. The feedback uses routinely collected data and also includes persuasive messaging, evidence updates and suggested action plans.
LAMP has helped general practices reduce antibiotic prescribing. For example, in Humber and North Yorkshire ICB overall antibiotic prescribed fell by 21.5% during 2023-24 whilst in West Yorkshire antibiotic prescribing for upper respiratory tract infection fell by 13.3% over 2022-3. Reducing antibiotic overuse protects these lifesaving medicines for future generations.
Greener prescribing of inhalers for asthma
Asthma affects nearly one in ten of both adults and children in the UK, making it one of the country’s most common long-term conditions. Despite this, the asthma mortality rate in the UK remains amongst the worst in Europe. Over-reliance on short acting bronchodilators (SABAs, usually salbutamol) as relievers is a significant risk factor for avoidable mortality. Furthermore, asthma inhalers alone account for around 13% of the NHS Primary Care carbon footprint. Sarah Alderson led the Campaign to Help Improve Respiratory Prescribing (CHIRP) across West Yorkshire. CHIRP promotes both more effective asthma treatment, in line with clinical guidelines, and prescribing of greener inhalers with lower global warming potential (especially dry powder inhalers). Since the campaign targeted the 268 general practices in West Yorkshire from 2023, 2440 fewer people with asthma were prescribed six or more SABAs in the preceding year and 933 fewer prescribed 12 or more SABAs in the preceding year.
Towards a learning health system
Paul Carder, Head of Research for West Yorkshire ICB, is co-leading this programme and commented that, “The feedback campaigns directly feed into two of the Health and Care Partnerships’ 10 Big Ambitions: to increase the years of life that people live in good health in West Yorkshire; and to reduce antimicrobial resistant infections. They also align with our ongoing Core20Plus5 responsibilities to address health inequalities within the region. Our established partnership with the ARC researchers demonstrates how to align real-world research with service improvement.”
Yorkshire and Humber ARC has demonstrated how to embed and scale up NIHR research findings on improving prescribing in general practice. Sarah Alderson is leading two further NIHR-funded studies with the ICB. Impact of an Intervention on Inequalities in Overprescribing (The 3i-o Study) will evaluate the impact, implementation and sustainability of audit and feedback on health inequalities in prescribing in general practice. Adapting and evaluating a complex adaptable intervention to reduce opioid prescribing in primary care (Opioid SMART) will optimise feedback to reduce prescribing of opioids for chronic non-cancer pain in primary care using a clustered, sequential, multiple-assignment randomised trial (SMART).
The partnership between the ARC researchers and West Yorkshire ICB represents an evolving learning health system, which integrates continuing improvement with rigorous evaluation.
Examples of excerpts from feedback reports

How has this made difference?
The programme has reached over 1,000 practices across Yorkshire and North East England, delivering significant improvements:
- Antibiotic Prescribing: 21.5 % reduction in overall antibiotic prescribing in Humber and North Yorkshire (2023-2024). 13.3 % reduction in antibiotic prescribing for upper respiratory infections in West Yorkshire (2022-2023)
- Asthma Care: 2,440 fewer patients prescribed excessive amounts of inhalers. 933 fewer patients prescribed very high amounts. Contributed to reducing the NHS primary care carbon footprint.
- Opioid Prescribing: 1.9% decline in overall opioid prescribing. 1.5% decline in strong opioid prescribing in South Yorkshire and Bassetlaw (2021-22)