by Rebecca M Simpson
Unsustainable levels of demand on emergency services are an international issue.1,2 Finding solutions to the problem of demand continues to be a focus of UK government policy.3 Demand placed on the urgent and emergency care system by children has not received the same attention as that placed by adults, despite the fact that children are higher users of Emergency Departments (ED) services.4 A large proportion of ED attendances in children may be non-urgent attendances, which could be better managed elsewhere.
In this study, we aimed to explore differences in non-urgent attendances and urgent attendances in children to ED and determine which children present in this way and when. This has been published in the Emergency Medicine Journal5 and cited in the recent policy report by the Royal College of Paediatrics and Child Health.6
We used a dataset extracted from the CUREd research database which contains data on the provision of care in Yorkshire and Humber from 13 hospitals.7 The data we used included ED attendance and admitted patient care for children aged 0-15 between April 2014 and March 2017. For the analysis of this data, we used summary statistics to describe the study sample and regression models to compare non-urgent attendances with urgent attendances. We were interested in whether there were any differences in age, mode and time of arrival, deprivation as well as waiting, treatment and total department times for non-urgent verses urgent attendances.
We defined a non-urgent attendance using a previously validated definition.8 This definition refers to all first-time attenders (not a follow-up attendance) to an ED who were then identified as not receiving any treatments, investigations or referrals which would require the facilities provided by an ED.
We found in our data that there were a total of 1,068,598 ED attendances from children across the 13 hospitals, between April 2014 and March 2017. Of these attendances, 91.5% (977,907) were a first-time attendance and of those, 21.4% (208,788) were classified as non-urgent attendances (figure 1).
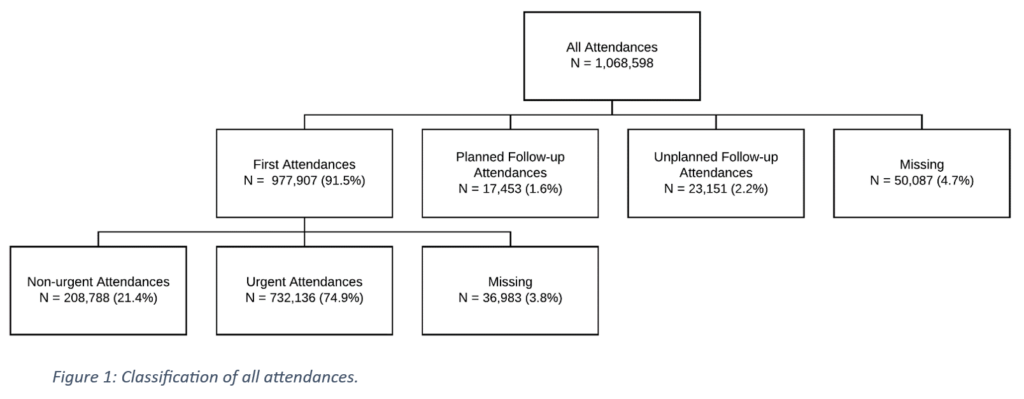
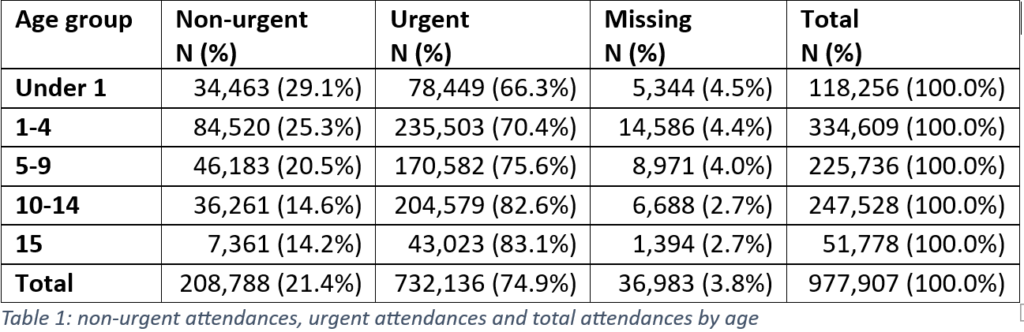
We found that the proportion for children attending ED with a non-urgent attendance decreased as aged increased, meaning a higher percentage of younger children attended ED for a non-urgent attendance (Table 1).
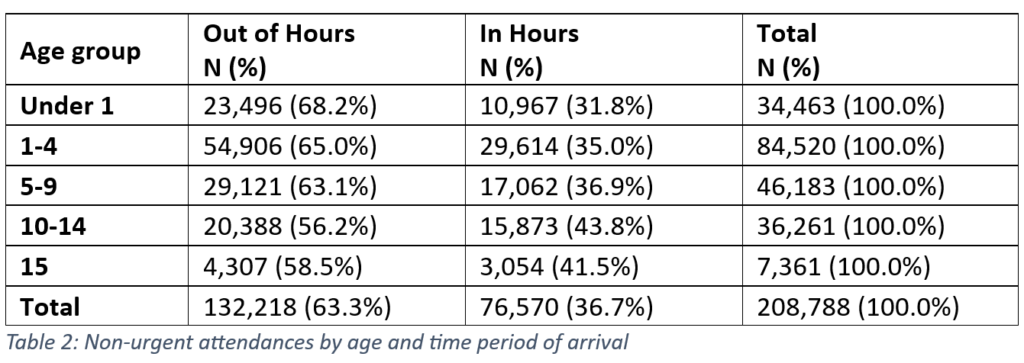
We also found that those who attended out of hours were more likely to be non-urgent when compared to those who attended in hours (In hours was as follows: 08:00–18:00, Monday–Friday).
The plots in figure 2 show shows the number of first-time attendances (figure 2 (top)) and the percentage of attendances that were non-urgent (figure 2 (bottom)) by day of week and time of day. There is a ‘double peak’ in numbers of first-time attendances across each day of the week, with the first at around midday and the second around 18:00 (start of out of hours). A similar ‘double peak’ pattern is seen Monday–Friday in the percentage of children who are non-urgent attendances, although at different time points, with a first peak in the early afternoon and the second, highest peak of non-urgent attendances around 23:00–01:00.
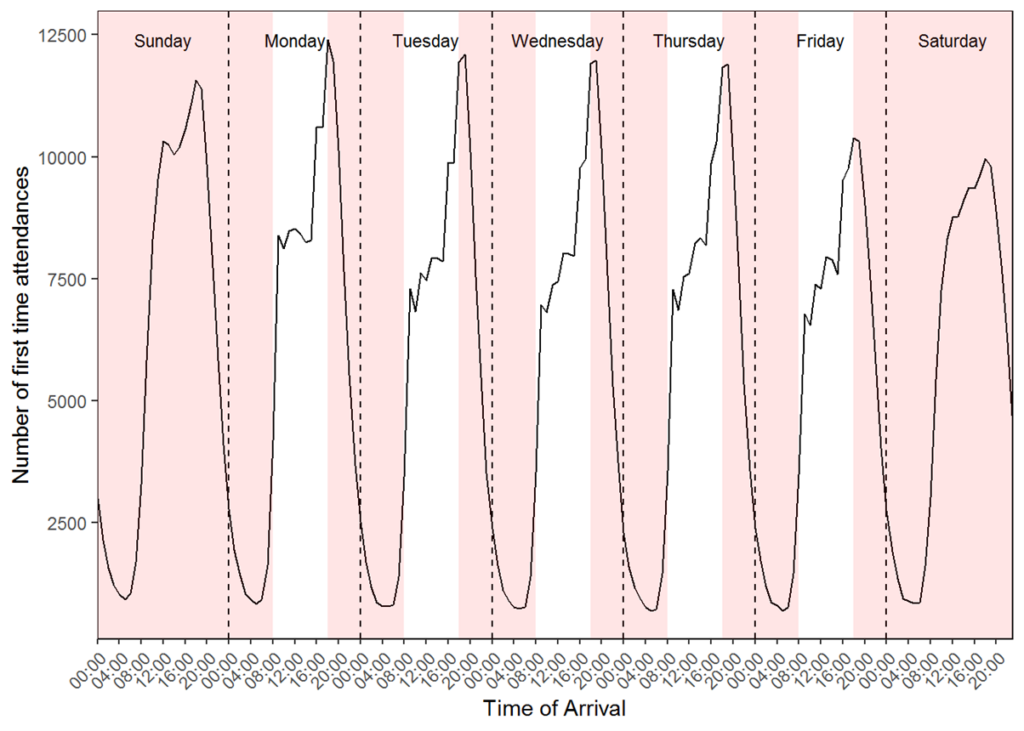
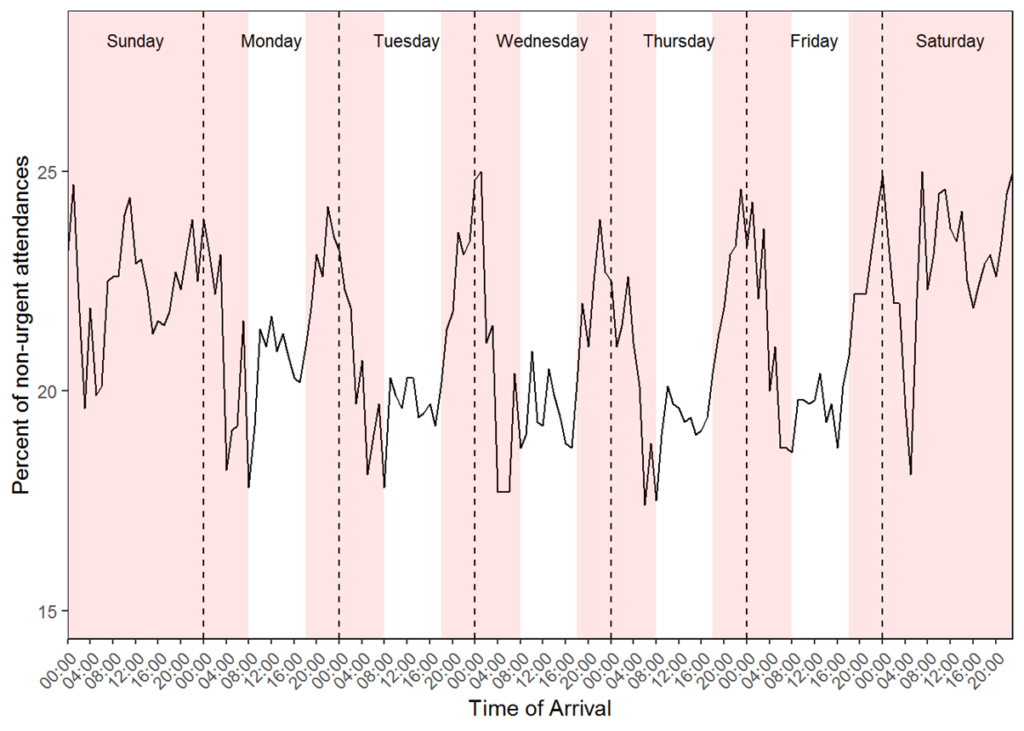
Figure 2:Proportion of all first-time attendances (top) and non-urgent (bottom) by day of the week and time of the day (red: out of hours).
We explored the relationship between age and out of hours for non-urgent attendances further and found that there was a higher proportion of non-urgent attendances for younger children attending out of hours compare to older age groups (Table 2).
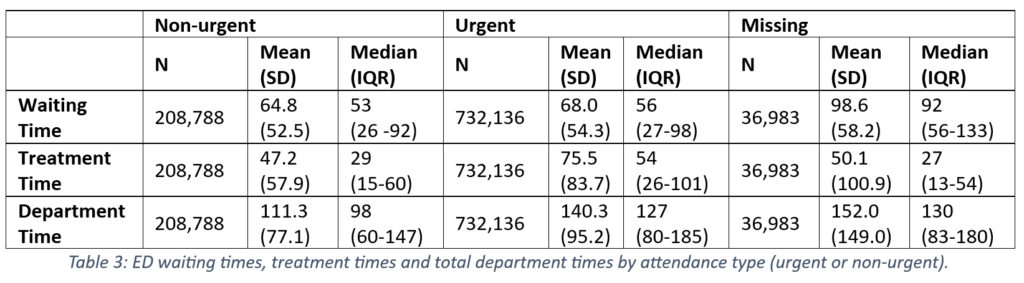
We also found that non-urgent attendances spent less total time in the ED, with a median (IQR) of 98min (60–147) compared with 127min (80–185) for urgent attendances (Table 3). This was consistent for all three time measurements, with non-urgent attendances having shorter times than urgent attendances. This means non-urgent attendances are seen more quickly.
Conclusion
We found in this study that a large proportion of ED attendances in children are non-urgent attendances. Non-urgent attendances were more likely to be children in the youngest age categories (<5 years) and out of hours. Non-urgent attendances are seen more quickly in ED across all time measures, with both mean and the median total time in department for non-urgent attendances well below the four-hour target, more so than for urgent attendances.
Our data suggest there are particular groups of children for whom targeted interventions would be most beneficial. Children under 5 years would be such a group, particularly in providing accessible, timely care outside of usual community care opening hours.
References
- NHS England. High quality care for all, now and for future generations: Transforming urgent and emergency care services in England – Urgent and Emergency Care Review End of Phase 1 Report, Appendix 1 – Revised Evidence Base from the Urgent and Emergency Care Review, 2013. Available: https://www.nhs.uk/NHSEngland/keoghreview/documents/UECR.Ph1Report.Appendix%201.EvBase.FV.pdf [Accessed 26 Aug 2021].
- Lowthian JA, Curtis AJ, Cameron PA, et al. Systematic review of trends in emergency department attendances: an Australian perspective. Emerg Med J 2011;28:373–7.
- NHS England. The NHS Long Term Plan, 2019. Available: https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/ [Accessed 26 August 2021].
- Keeble E, Kossarova L. Quality Watch. Focus on: Emergency hospital care for children and young people. What has changed in the past 10 years? Research report, 2017. Available: https://www.nuffieldtrust.org.uk/files/2018-10/1540142848_qualitywatch-emergency-hospital-care-children-and-young-people-full.pdf [Accessed 26 August 2021].
- Simpson RM, O’Keeffe C, Jacques RM, et al. Non-urgent emergency department attendances in children: a retrospective observational analysis. Emerg Med J 2022;39: 17-22. doi:10.1136/emermed-2021-211431
- Jenkins S, Firth A, Cheung R, McKean M, Turner, S. From left behind to leading the way: a blueprint for transforming child health services in England. 2024.London (UK): Royal College of Paediatrics and Child Health.
- Mason S, Stone T, Jacques R, et al. Creating a Real-World Linked Research Platform for Analyzing the Urgent and Emergency Care System. Medical Decision Making 2022;42(8): 999-1009. doi:10.1177/0272989X221098699
- O’Keeffe C, Mason S, Jacques R et al. Characterising non-urgent users of the emergency department (ED): a retrospective analysis of routine ED data. PLoS One 2018; Feb 23;13(2).