by: Pip Shaw1, Eloise Ryde2, Julie Blanchard3, Gary Hellewell3, Colin Lewisohn3, Alison Potts3, Angie Ross3, Irina Sidorova

This blog outlines research carried out by University College London and ARC Yorkshire & Humber. We investigated how health professionals worked together to set up and deliver a new approach to care for people with complex mental health conditions.
We have purposefully used ‘complex mental health conditions’ in this blog rather than ‘severe mental illness’, the preferred phrase we decided on during discussions with service users and carers.
Background
Research tells us that joined-up care for mental and physical health is the best way to support patients, but patients don’t always receive integrated care as needed. This could signal there are challenges to getting integrated care set-up and delivered.
Therefore, we decided to research how some updated care guidelines, Primrose, were implemented. Primrose was created by researchers in collaboration with service users, carers and health professionals, and has been shown to improve patients mental and physical health as well as save the NHS money.
The updated guidelines encouraged health professionals from primary care, secondary care, and the voluntary sector to work together to provide tailored care for people with complex mental health conditions.
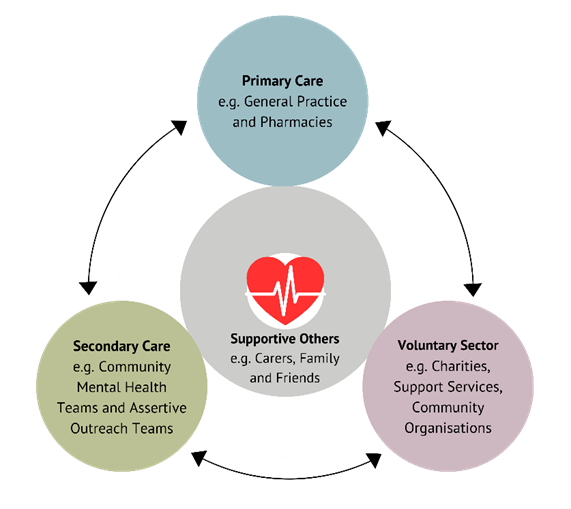
Figure 1: How Primrose will join up care for patients
What was being set up?
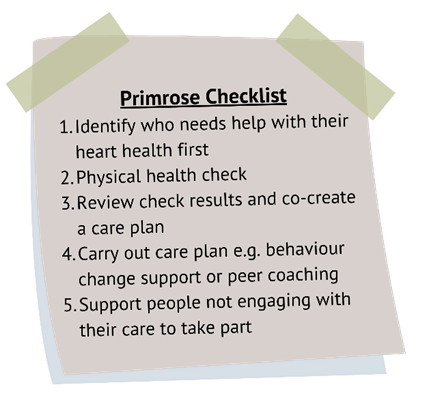
Figure 2: The five key elements of Primrose
Primrose is an evidence-based set of guidelines around providing comprehensive and personalised care. It was developed to support patients with complex mental health conditions at risk of, or those who have, poor heart health.
Primrose was created because people with a diagnosis of complex mental health conditions are more likely to develop conditions of the heart and blood vessels.
When risks or potential risks of poor heart health are identified, for example high blood pressure, teams of health professionals can intervene to support patients to reduce this risk. This support is tailored to each patient’s needs and what is important to them – e.g. reviewing medication options, support sessions for lifestyle change (e.g. eating healthier), peer coaching, and signposting for additional concerns like housing
This support is tailored to each patient’s needs and what is important to them – e.g. reviewing medication options, support sessions for lifestyle change (e.g. eating healthier), peer coaching, and signposting for additional concerns like housing.
What were we researching?
To meet our aims we wanted to know what worked well and what didn’t when setting up Primrose, to help understand how to implement joined-up care and continue successful delivery of Primrose.
To develop this understanding, we looked at how Primrose was set-up including the decisions and processes involved. We consulted with service users and carers to shape the design of the research which identified gaps in services they had received.
We therefore attended decision making meetings, visited General Practices, interviewed health professionals (e.g. GPs, nurses, and peer coaches), and understood how the care was currently being delivered, for example which health professionals were involved at each step.
What did we learn?
Over the last two years key findings were:
- Setting up Primrose in 24 General Practices was challenging but achievable and helped to improve coordination between General Practices in primary care, secondary care, and the voluntary sector (Figure 1).
- Success was achieved through strong leadership at every level, excellent cooperation, and through utilising the Primrose approach; giving health professionals time to learn, reflect, and solve problems.
- However, challenges across the NHS system made things harder—such as difficulties connecting digital health records, limited staff capacity, and a culture that focused more on screening for risk rather than taking action to improve the health and wellbeing of patients with complex mental health conditions.
What does this mean?
From these findings, this is what we are going to recommend to teams of health professionals and policy makers (e.g. members of parliament) to achieve stated government policy:
- Prepare the NHS system: Make it easier to introduce evidence-based new approaches like Primrose by improving connections between health professionals working across primary care, secondary care, and the voluntary sector (such as digital health records) and educating health professionals to support both the physical and mental health of patients with complex mental health conditions.
- Adapt to local needs: When using Primrose, tailor it to fit existing local services (across primary care, secondary care, and the voluntary sector). Health professionals also need ongoing training, time to reflect, and support to overcome challenges.
- Build strong teams: Having a committed team of health professionals —including leaders who understand Primrose and its importance—can help us all ensure better joined-up care to improve the health and quality of life for patients with complex mental health conditions.
At the end of the research, teams of health professionals across the 24 General Practices continue to deliver Primrose. Primrose is an approach to better support patients with severe mental illness at risk of, or who have, poor heart health, which also saves the NHS money and encourages joined-up care. We hope new teams of health professionals take up these recommendations and Primrose to make sure patients with complex mental health conditions get better and more efficient health care.
1 University College London
2 Bradford Teaching Hospitals NHS Foundation Trust
3 The DIAMONDS Patient and Public Engagement panel
Contact: philippa.shaw@ucl.ac.uk